Campus News
Biophysicist David Kliger investigates how a protein goes wrong and causes blindness
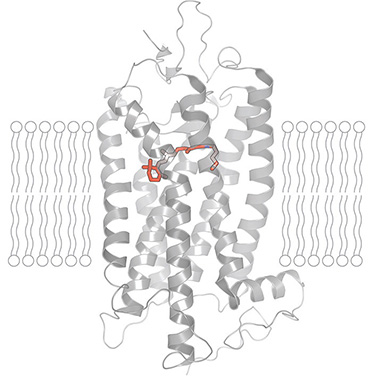
Abnormal versions of the protein rhodopsin lead to blindness in people with the genetic disease retinitis pigmentosa.
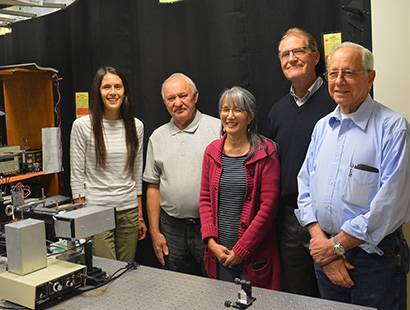
David Kliger, a distinguished research professor of chemistry and biochemistry at UCSC, has received new funding from the National Institutes of Health (NIH) to help unravel the molecular mechanisms in the disease retinitis pigmentosa.
An inherited disease that leads to blindness, retinitis pigmentosa can be caused by mutations in the gene for rhodopsin, a light-sensitive protein found in the retina of the eye.
Kliger’s lab has been studying rhodopsin for the past 40 years. With the recent funding, part of a larger grant awarded to Oregon Health & Science University (OHSU), Kliger will investigate how the mutated, or abnormal, rhodopsin protein behaves differently from the normal protein.
Kliger first became interested in retinitis pigmentosa when a colleague’s wife began to experience early symptoms associated with the disease. “It’s a gradual degenerative change,” he said, noting that those affected by mutations in the rhodopsin gene lose their eyesight gradually as cells die off in the retina, the light-sensing tissue at the back of the eye.
Motivated by a personal tie to the disease and determined to be a part of the effort to find a solution, Kliger set out on a multi-decade journey. At the time, little was known about how the mutations change the functioning of the rhodopsin protein.
Rhodopsin is found in the retina’s rod cells, which are responsible for vision in low-light conditions. Rods and cones, the other type of light-sensing cells in the retina, convert light into electrical signals that get sent to the brain by the optic nerve. Rhodopsin plays a crucial role in this process. When light enters the eye and hits the rhodopsin, it causes small movements within the protein’s structure that set off a cascade of reactions leading to an electrical impulse that eventually registers as sight.
Retinitis pigmentosa
In retinitis pigmentosa, mutations in the gene for rhodopsin result in an abnormal version of the protein that doesn’t work correctly and eventually causes the rod cells to die. Over time, the loss of the rod cells causes cone cells to die as well, resulting in blindness. Different mutations in the rhodopsin gene are associated with different rates of progression and age of onset of the disease.
In order for Kliger and his team to understand the abnormal rhodopsin, they first needed to understand the functioning of healthy rhodopsin as it responds to light at near-physiological temperatures. Prior research on this process had been done at low temperatures to slow down the protein’s movements. Kliger and his team set out to document the steps rhodopsin goes through at room temperature. The sophisticated equipment and technology needed for this work didn’t exist yet, so they built their own.
“It’s hard to imagine how much work it was to get to this point,” Kliger explained. “We were having to solve one problem that then led to another problem, which led to another.”
After decades of research, Kilger and his team have pioneered a new way to “see” rhodopsin and how it changes shape as it interacts with light. The technique they use—nanosecond time-resolved spectroscopy—enables them to deconstruct the steps in the process by analyzing the changes in the color of light that is absorbed as it passes through the rapidly morphing proteins. This work has enabled Kliger’s team to uncover several previously unknown steps in the functioning of rhodopsin.
Finally equipped with a roadmap of how healthy rhodopsin behaves when exposed to light, Kliger can now begin to investigate what goes wrong in retinitis pigmentosa. “Now we’re in a position to ask what exactly happens when you have a mutation in the protein that causes a disease,” he said.
Under the new NIH grant, Kliger’s team will be collaborating with a team led by David Farrens at OHSU. Their goal is to analyze abnormal rhodopsin in the same way they did with the healthy proteins and compare the results.
“We want to look at the mechanism and figure out where it stops working,” Kliger said, adding that he is hopeful this work will enable the development of targeted therapies for treating retinitis pigmentosa.
Although the woman who initially inspired Kliger and his team to embark on this journey has now essentially lost her eyesight, he remains dedicated to the cause. “Without knowing what is happening, it’s hard to know what we’ll have to do to overcome it,” he said, “but we’re as close as we’ve ever been.”