Campus News
Light-induced delivery of nitric oxide eradicates drug-resistant bacteria
UCSC researchers have developed a novel approach for eradicating drug-resistant bacteria from wounds and skin infections, using light to trigger the controlled release of nitric oxide.
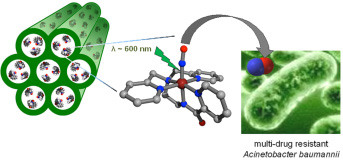
Researchers at UC Santa Cruz have developed a novel approach for eradicating drug-resistant bacteria from wounds and skin infections, using light to trigger the controlled release of nitric oxide. The UCSC team developed a photoactive compound that releases nitric oxide when exposed to light, and loaded it into a porous, biocompatible material that could be applied as a sprayable powder.
In laboratory tests, the light-triggered nitric oxide treatment eradicated a highly drug-resistant strain of Acinetobacter baumannii, a type of gram-negative bacteria that causes hard-to-treat and potentially lethal infections throughout the world, including serious infections in soldiers wounded in Iraq and Afghanistan. The team led by Pradip Mascharak, professor of chemistry and biochemistry at UC Santa Cruz, and graduate student Brandon Heilman published their results in the Journal of the American Chemical Society (JACS). The paper is currently available online and will be featured on the cover of a future print issue of the journal.
Nitric oxide has potent antimicrobial effects and is known to play a role in the immune system and promote wound healing. Gaseous nitric oxide has been used to treat infected wounds, but handling the toxic and reactive gas poses many challenges. So researchers have begun exploring a variety of other methods for delivering nitric oxide as an antibiotic treatment. Because nitric oxide attacks a large number of targets in microorganisms, including DNA, proteins, and lipids, many scientists expect bacteria will not easily develop resistance to it.
Mascharak’s lab developed a photoactive manganese nitrosyl, a compound that rapidly releases nitric oxide when exposed to light. As a carrier for this compound, the researchers used a porous silicate material known as MCM-41, which traps the photoactive compound inside its pores. They also tested a related aluminosilicate material (Al-MCM-41), which holds the photoactive compound even more tightly. Tests showed that after the light-triggered release of nitric oxide, the byproduct of the reaction remains trapped inside the powdery, biocompatible material.
“It only delivers nitric oxide. The rest remains trapped in the material, which can be washed out of the wound,” Mascharak said. “We think it could be used as a sprayable powder for treating battlefield wounds.”
Acinetobacter baumannii has earned the nickname “Iraqibacter” because it has caused so many serious infections in soldiers wounded in Iraq. Some strains of the bacteria are resistant to virtually all antibiotics. Mascharak’s lab tested their compound against a strain, isolated from a soldier injured in Afghanistan, that showed resistance to nine of 11 antibiotics tested.
To test the photoactive compound, the researchers developed a laboratory model of skin and soft-tissue infections. A standard antibacterial assay involves growing bacteria on the surface of an agar plate (a petri dish with a layer of firm, gelatin-like growth medium). In an infection, however, bacteria are not only on the surface but also deeper within the skin or soft tissues. “We realized that there wasn’t a good model for in vitro testing of antibiotics against soft-tissue infections,” Heilman said.
To more closely mimic the conditions in an infected wound, Heilman mixed bacteria into a warm solution of “soft brine agar” and poured that onto agar plates to solidify. The bacteria then grew throughout a 1.1-millimeter-thick layer of soft agar, allowing growth and colonization to occur in a manner similar to that seen in skin and soft-tissue infections.
Heilman then applied the aluminosilicate powder, with and without the photoactive manganese nitrosyl compound, to a defined area of the plates before shining visible light on them. The released nitric oxide effectively cleared the bacteria from the treated areas of the plates, showing that the nitric oxide easily penetrated through the agar layer. The amount of light used to activate the compound (100 milliWatts per square centimeter) is a typical light flux on a sunny day, Mascharak said.
The ability to control the release of nitric oxide using light is a significant advantage for clinical applications, he added. Tests showed that illumination of the material causes a steady release of nitric oxide, which can be stopped and started repeatedly by turning the light off and on. In the field, this could be accomplished by covering and uncovering the treated area.
“This is the first proof-of-concept to show that it works,” Mascharak said. In the paper, the researchers concluded that “It is expected that application of these nitrosyl-containing porous materials to infected wounds followed by exposure to sunlight will bring about a rapid reduction of the pathogen load.”
The researchers now hope to find collaborators who can help them with the next levels of testing needed to develop the clinical potential of their compound.
In addition to Heilman and Mascharak, the coauthors of the paper include Jessica St. John, a UCSC graduate student, and Scott Oliver, associate professor of chemistry and biochemistry, who helped with the characterization of the materials. This research was supported by the National Science Foundation and the California Institute for Quantitative Bioscience (QB3).