Campus News
Uncovering the politics behind a pandemic
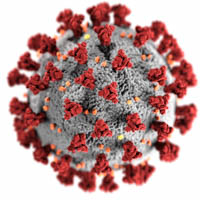
The latest paper from Politics Professor and Global & Community Health Executive Director Matt Sparke argues that the coronavirus pandemic has exposed, exploited, and exacerbated the vulnerabilities of neoliberal societies around the world.

The latest paper led by UCSC Global & Community Health Executive Director and Politics Professor Matt Sparke points to neoliberalism as a contributor to the causes and impacts of the coronavirus pandemic. Sparke and his coauthor, health policy researcher Owain Williams, gather findings from a global body of social science and public health research in their article “Neoliberal disease: COVID-19, co-pathogenesis and global health insecurities.”
Neoliberalism is an approach to government that prioritizes free-market capitalism, and its focus on market-based freedoms, rules, and incentives has become dominant around the world since the 1970s. Though neoliberalism is commonly thought of as being associated with growth and freedom, Sparke says neoliberal goals often come at the expense of societal well-being and freedom from vulnerability. The coronavirus pandemic has made this especially clear, he argues, and the paper explores that concept.
“A lot of people look at COVID as a set of symptoms that expose underlying social problems, and we agree with those arguments,” Sparke said. “We’re adding to that an overview and analysis of the multiple pathways through which this has happened. The virus has gone down these rifts through neoliberal society and actually exploited and exacerbated them.”
In particular, the paper makes the case that neoliberalism has transformed health care, through privatization and commodification of goods and services in place of public investment in social programs and health systems. Sparke and Williams argue that this set the stage for the virus to spread by exploiting vulnerabilities in marketized healthcare and the wide lack of social protections. The paper also traces some of the virus’s disparate impacts on marginalized communities back to the intersecting damage done by pro-market policies in neoliberal societies.
Coronavirus transmission exploits social vulnerabilities
The paper describes neoliberalism as having “hollowed out” national and global health organizations over time, resulting from systematic defunding coupled with policies of contracting out services to private firms. Sparke and his coauthor contend that these trends left public health systems without the institutional or bureaucratic capacity to manage a response to the coronavirus pandemic effectively.
The paper also says that for-profit models in hospitals and health-care product supply chains failed under the strain of the pandemic, resulting in health-care worker layoffs, hospital closures, and price gouging that limited care and treatment options for some patients.
At the same time, de-unionization and decades of disinvestment from social welfare programs left many workers around the globe without reliable job and income protections or support for housing and health during the pandemic, the paper argues. Sparke and Williams say this meant that low-paid “essential workers” had little choice but to face risk of infection under working conditions that aided the virus’s spread.
In long-term care homes for the elderly, for example, Sparke says low pay and lack of job stability has led many care workers to work multiple jobs to make ends meet, and they often don’t have sick leave, which means they may show up for work even when they’re not feeling well. The paper says these conditions essentially turned workers into carriers for disease and allowed the virus that causes COVID-19 to spread easily among nursing homes.
“The way that issue has most often been represented in public is, ‘Well, people living in nursing homes are vulnerable because they’re elderly,’” Sparke said. “But really, it’s also because they’re being cared for by extremely exploited workers who do not get sick leave and who have to work multiple jobs. And that’s a very clear example of how the neoliberal labor market norms became integral to the spread of the virus.”
Pandemic impacts exacerbate inequality
The paper also argues that neoliberalism contributed to disparate pandemic impacts that deepened social inequities and vulnerabilities in societies where market rule is most advanced. In the United States, for example, health insurance is most often linked to employment, and health care operates as a commercial enterprise, which the paper says led to wealthy, gainfully employed individuals having better access to health insurance, health facilities, providers, and health-care products during the pandemic.
Meanwhile, marginalized groups faced increased risk of serious illness and death. The paper points to the example of research led by new UCSC Assistant Professor of Sociology Alicia Riley, which found that the first seven months of the coronavirus pandemic disproportionately impacted mortality among Latino immigrants in California, especially those in unprotected, essential jobs.
The paper also contends that pharmaceutical company business models limit global vaccine access for low-income countries. Sparke and Williams describe intellectual property rights as creating “paywalls” and other obstacles to vaccine access, where wealthy countries protect the patent monopolies of pharmaceutical companies, and low-income countries are left to rely on philanthropic efforts that often fail to deliver.
Sparke says this pattern remains true for the COVAX campaign, administered by the Global Alliance for Vaccines and Immunizations, despite some extraordinarily generous gifts from individuals and foundations.
When viewed together, Sparke believes the wide range of inequities produced by market-stratified societies and privatized health care during the pandemic show that the goals of public health and neoliberalism are often pointed in opposite directions.
“The market has been very successful at things like advancing the interest of intellectual property for firms and the profit of care homes, and those are successes in the market’s own very narrow terms, but they’re failures in moral, health, and social terms,” he explained. “There’s a tendency to present this as an area of so-called ‘market-failure’, but in reality, market successes are leading to huge social and health failures.”
Toward a new vision for public health
Sparke and Williams ultimately argue that the harms of the coronavirus pandemic result from multiple factors working together. Those factors include biological elements, like the characteristics of the virus itself, as well as other vulnerability-producing social forces, such as racism. But they can also stem from market-made social inequalities produced by neoliberalism.
“Looking back through history, this pandemic is not the only example of disease enabled by neoliberalism, and we also don’t think this will be the end of it,” Sparke said. “But we do hope that it would be helpful for the pandemic rebuilding process if neoliberalism was at least identified as part of the problem.”
Sparke says better responses to future health crises—and more proactive policies to promote public health—will require integrated approaches that consider biological and social factors together.
“That approach is very much at the heart of how we are designing our Global and Community Health undergraduate programs at UC Santa Cruz,” he said. “Natural scientists, social scientists, engineers, and arts and humanities scholars will all come together to provide our students with an integrated bio-social analysis of health challenges and possible ways of addressing them.”